The administrator in the Controller’s area was hospitalized two weeks ago after being diagnosed with meningococcal meningitis serogroup (strain) C and is “recovering nicely,” according to University personnel.
The employee is currently “doing great” and is anticipated to be moved out of the intensive care unit (ICU) to a “stepped down unit,” according to Patti Swannack, the Vice President for Administrative Services. She said the family members of the patient are also fine.
President Dr. Paul R. Brown sent an email on Thursday, Nov. 21 alerting the campus community of the University employee infected with meningitis. It stated in the email, “The employee, who is an administrator in the Controller’s area, is gravely ill and has been admitted to a hospital.”
Director of Health Services, Kathy Maloney said the identity of the employee will not be disclosed to maintain his/her privacy and confidentiality.
“The University has been in touch with officials from both the Monmouth County Regional Health Commission and the New Jersey State Department of Health,” said Mary Anne Nagy, Vice President of Student and Community Services. Officials have also been in contact with the Center for Disease Control (CDC).
“The University took precautions when we were first informed of the situation,” said Swannack. “We brought in the University’s Consulting Physician, Dr. Robert Hershkowitz, and Kathy Maloney … to meet with and speak to our employees. We also thoroughly cleaned the offices where the employee worked.”
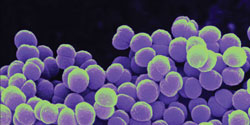
According to CDC.gov, “Meningitis is a disease caused by the inflammation of the protective membranes covering the brain and spinal cord known as the meninges. The inflammation is usually caused by an infection of the fluid surrounding the brain and spinal cord.”
Meningococcal meningitis occurs in people of all ages but it is more common in infants, young children and the elderly. However, college students and military recruits are at a slightly higher risk because of their living conditions, according to the New Jersey Department of Health.
The CDC said meningococcal meningitis is caused by a type of bacteria called Neisseria meningitidis, also known as meningococcus, and is spread through the exchange of respiratory and throat secretions, such as like saliva. This means that the person who may catch the disease must be in close contact with the person infected, according to the New Jersey Department of Health.
The New Jersey Department of Health explains this type of close contact as living in the same household or sleeping in the same home, kissing, sharing eating utensils or food, sharing drinks or cigarettes and uncovered face-to-face sneezing or coughing.
“It is an extremely difficult disease to transfer, unless you have been exposed for eight or more hours within three feet of the infected person,” said David Henry, Monmouth County Regional Health Commission Health Officer. He added that the casual contact or the breathing of air with a person with meningoccal disease will not spread the bacteria.
The bacteria cannot be spread by casual contact such as being in the same room as the infected person or touching something that the infected person has touched, according to the New Jersey Department of Health.
“[There is] no rhyme or reason as to who it strikes and when it strikes,” said Maloney.
The University held an information session on Nov. 21 in Pollak Theatre after the community was informed about the ill employee. Brown explained that the reasoning for holding this information session was to educate the University community about the most recent health concern. “So many of our colleagues are collaborating together and trying to make sure we absolutely keep a safe and healthy work environment,” he said during the conference.
Henry, Maloney, Brown and Nagy attended the information sessions along with other administrators who were willing to answer any questions asked and address any concerns. Brown said that the University wished to be as “transparent” as possible regarding the situation. “[We want to] make sure we are absolutely on top of this,” he said while opening the information session.
One question asked was if it was possible that someone could be a carrier of meningitis without ever becoming ill. Maloney responded with “absolutely.”
Approximately 10 percent of people have Neisseria meningitis bacteria in the back of their nose and throat with no signs or symptoms of disease, classifying these people as being “a carrier,” as explained by CDC.gov.
Maloney said the ill employee experienced initial symptoms on Nov. 18. Symptoms include sudden onset of fever, headache, and stiff neck often accompanied by other symptoms including nausea, vomiting, sensitivity to light, and an altered mental state.
According to Maloney, the incubation period is approximately ten days. Therefore, it can be inferred the employee was contagious from Nov. 8 to Nov. 18. “I feel comfortable that it hasn’t spread … and we are carefully monitoring the situation.”
The diagnosed strain in the employee is one of the common forms of meningitis and is covered under the vaccine issued for use in the United States.
Students living in University owned or sponsored housing are required to get the meningitis vaccination and they must provide proof of immunization before attending the University, said Swannack. She explained that it is not required by state law that commuter students receive the vaccination but the University does recommend it.
However, this is not the case with employees. It is not recommended by the CDC that faculty members get the vaccination, according to Swannack.
Maloney said that since meningitis is more at risk for young adults, the vaccination is required for them but not for older people. “College students die every year from bacterial meningitis,” she said.
CDC.gov explained the vaccine students routinely get protects against four serogroups known as A, C, Y, and W, but not against B. The case of meningitis found at the University differs from Princeton University (PU), where eight cases of serogroup B meningoccal meningitis have been identified since March.
Students and faculty at PU are recommended the vaccine for serogroup B that is licensed for use in Europe and Australia but not the United States. As stated on Web.Princeton.edu, “The CDC and the Food and Drug Administration have allowed the use of this vaccine for this particular situation at PU.”
The CDC, which according to Henry did not get involved with PU until the sixth confirmed case of meningitis, is allowing Maxim Health Systems to administer the vaccines. Maxim Health Systems also runs the annual flu vaccine clinic on PU’s campus. Henry was the health advisor at PU up until this past September.
When asked what advice PU has to offer other institutions dealing with meningitis, PU Media Specialist Michael Caddell said, “Our position is that each institution will make its own policy decisions based on what suits specific needs or concerns, and the types of general comparisons yielded from contacting multiple institutions are not constructive.”
Brown said, “We are benchmarking with Princeton. We must be very vigilant about our health.”
“I think meningitis is overlooked and is not taken as seriously as it should,” said Patricia Fontaine, a senior health studies major. “It is contagious [and] if not treated early can have negative consequences.”
Quick medical attention is extremely vital if meningococcal meningitis is suspected. “If symptoms appear, get medical attention as soon as possible,” said Henry. He explained that most people with meningococcal meningitis are hospitalized and treated with antibiotics. “Most people don’t survive, and those who do have major complications,” he added.
Meningoccal meningitis can be prevented by getting vaccinated with meningococcal polysaccharide vaccine (MPSV4) and meningococcal conjugate vaccine (MCV4), which together are about 90% effective in protecting against the four strains, according to CDC.gov. Other defense mechanisms include practicing good public hygiene such as frequent hand washing as well as getting plenty of rest.